This essay is reproduced here as it appeared in the print edition of the original Science for the People magazine. These web-formatted archives are preserved complete with typographical errors and available for reference and educational and activist use. Scanned PDFs of the back issues can be browsed by headline at the website for the 2014 SftP conference held at UMass-Amherst. For more information or to support the project, email sftp.publishing@gmail.com
Danger: Women’s Work
by East Bay SftP
‘Science for the People’ Vol. 12, No. 2 March-April 1980, p. 6-12
This article was put together by a group of East Bay SftP members (Liz Katz, Steve Lyons. Sandra Marburg, and Jim Tobias). They wrote parts of it themselves and also incorporated articles by Jeanne Stellman of the Women’s Occupational Health Resource Center in New York (who generously allowed her work to be liberally edited) and material on clerical work hazards provided by Union WAGE (Women’s Alliance to Gain Equality).

Why is it necessary to separate the occupational health hazards of women from those of men?
• Because women are biologically different?
• Because women can pass on health hazards to fetuses?
Why are more women entering the job market?
• Because fewer women are becoming mothers?
• Because modern women have more free time?
We shall look at each of these questions in turn, and attempt to separate myth from reality. We shall then examine three occupations in depth: women health workers, clerical workers, and blue collar workers.
Occupational Health Hazards: Separate But Equal
Most scientists who conduct statistical studies on women’s occupational health feel it is necessary to separate women’s health hazards because women who are pregnant can potentially transfer those health hazards to the fetus. This by all means is a consideration. However, it is time that women stop being viewed primarily in terms of their childbearing capabilities. It is time that women’s occupational health, not simply pregnant women’s health, be studied and dealt with.
Obtaining information on women’s occupational health hazards is difficult. Examples of sexism in the study of women’s health hazards are numerous: the first major scientific conference on women’s occupational health, “Women and the Workplace,” held in 1976, dealt solely with health hazards in terms of reproductive capabilities. In 1963, a survey conducted by the U.S. National Center for Health Statistics on the effects of employment on pregnancy gathered only data on the occupation of the father; the mother’s job and job history were not even recorded! And the list goes on.
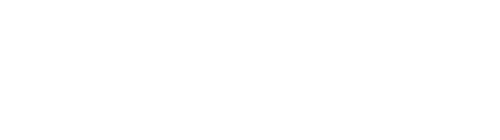
Women’s occupational health hazards must be studied separately from men’s because the majority of women have been coerced into very narrow areas of employment, as shown by the fact that the top 57 female occupations cover about 75 percent of all the women who work outside the home. However, the top 57 male occupations only cover 52 percent of all the men who work. Most readers could probably guess what the top ten job categories are for women: secretary, waitress, registered nurse, elementary school teacher, cashier, stitcher and sewer, retail salesperson, typist, private household worker, and bookkeeper.
Many excellent books and articles have been written on why and how women have been segregated into such narrow job categories, and we will not deal with that issue here. It should be noted, however, that most females find themselves in jobs in which they fulfill the role placed upon them by a male-dominated society — that of nurturer, supporter, and homemaker.
WHY ARE MORE WOMEN WORKING?
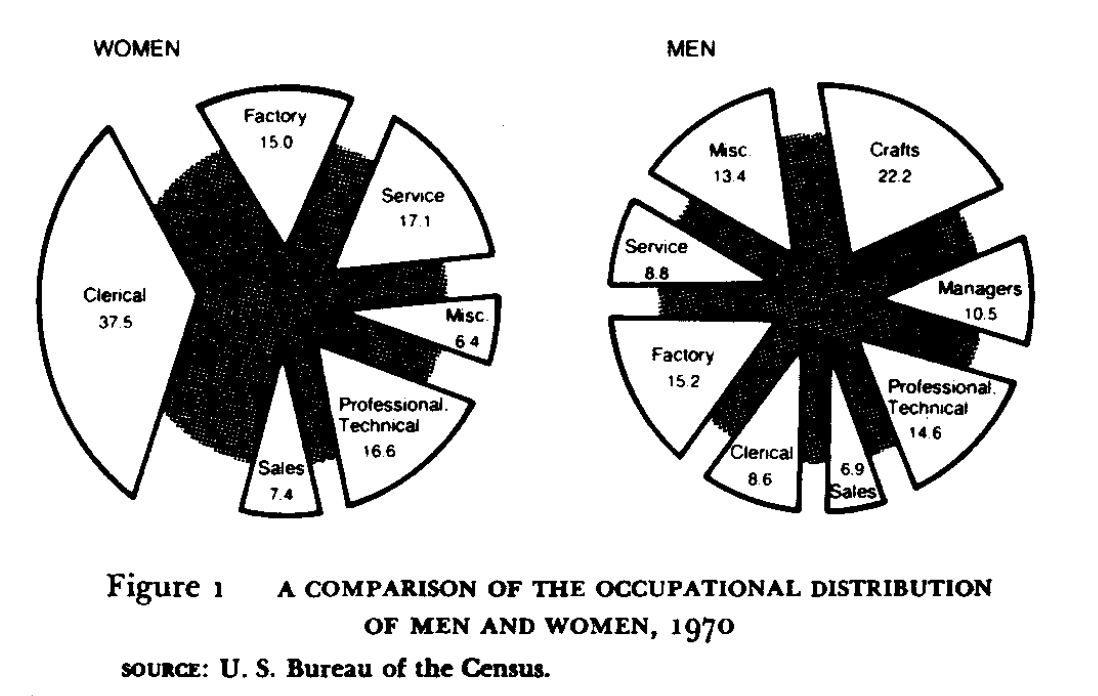
Figure 2 shows the percentage of women in the work force for the past 80 years. Why such a dramatic increase in the percentage of women working? The answer to this question is usually given in terms of a woman’s reproductive capabilities, aptly summarized in the following statement, from the U.S. Department of Labor Women’s Bureau’s “1975 Handbook on Women Workers”:
A series of technological and business innovations early in the century provided less costly substitutes for the manual work performed by women in the home. Perhaps even more significant was the dramatic change in child-related aspects of a woman’s life. For example, in 1910 married women in the age group of 45 to 59 years had borne an average of five children; by 1950 the number of children borne had declined to about half that figure.
The pieces seem to fit together, and the theory represents conventional wisdom on the subject of why women are working: an increase in free time due to technological and business innovations and decrease in family size. Again we see women viewed as childbearers and homemakers. However, as we shall see, this view is vased on an incomplete study of the statistics.
Fewer Children, More Mothers
To determine the increase or decrease of women free from the responsibilities of motherhood, it makes sense to look at the percentage of women who become mothers — as opposed to family size, as the Women’s Bureau has done. From this perspective, we find that although family size is decreasing, the percentage of women who are mothers is increasing! The percentage of women having no children has actually dropped from one in five before 1950, to about one in ten women today. Moreover, the greatest increase in women workers has been among women with young children. Thus to attribute the increase in women workers to smaller family size is false, because smaller family size does not, as we have seen, necessarily imply an increase in the number of women available to join the work force.
Increased Free Time?
Perhaps the explanation for why more women are working is that the amount of housework is decreasing, as the Women’s Bureau suggests. It would seem obvious that the amount of housework would decrease with the use of modern appliances and conveniences. However, the time spent at housework by most women today has actually increased by 6 hours a week since 1950 (70 hours a week compared to 64 hours a week).1 A decrease in household chores cannot therefore be the explanation for the increase in the number of women working for pay.
Why Are Women Entering the Labor Force?
Women and men work for similar reasons: economic need, economic independence, desire to own material goods, erosion of family earnings by rapid inflation, increased consumer debt at very high interest rates, identification of individual and social worth derived from a paycheck, and so on.
In 1978, over 42 million women were in the labor force as full-time and part-time workers. Forty per cent of these women workers were either single, widowed, separated, or divorced. This would suggest that most of these women worked to support themselves and possibly dependents. Women whose husbands earned less than $10,000 accounted for 7.2 million working women in 1978. In all, the U.S. Department of Labor estimates that nearly two-thirds of the women in the labor force in 1978 worked to support themselves and their families, or to supplement low family incomes.2 Finally, most women are not entering into the so called “glamorous” high paying jobs, but are entering as clerical workers, factory workers, and service workers at the lower ends of the pay scale.
STRESS: The Occupational Hazard Of the Dual Role for Women
In the majority of households, working women must bear the burden of both homemaker and breadwinner, the reason being that men do not share equitably in the housework. The old saying “a woman’s work is never done” has never been more true than it is today. On the average, working women are occupied at least 80 hours per week by their jobs and their homes, while working men average about 50 hours a week. For low income families, the inability to buy support services may place more stress on the woman to meet all the needs of the family, but even among high paid women workers the stress of the dual career is present. A recent study of female physicians in Detroit revealed that three out of four of these women did all the family cooking and shopping, and were responsible for child care as well. Moreover, about half of these women were married to physicians.
The result: women are faced with a work/home induced increase in psychological and physical stress. Stress causes complex changes in blood chemistry, digestive function and cardiovascular function, which over a long period of time may cause heart disease, kidney disease, stomach ulcers and ulcerative colitis. However, even though women are faced with ever increasing stress, almost all research money for cardiovascular research goes to the study of males.
WOMEN AND THE WORKPLACE
We have chosen to detail workplace hazards for three job categories in which women predominate: health care, clerical, and factory workers. These are not the areas in which job hazard may be greatest but rather the areas in which a large number of women are affected. We don’t know whether the health hazards in these jobs affect women differently than they affect men, because research has not addressed this question. We will not be discussing women’s health hazards in terms of hazard to fetuses. Rather, we will emphasize hazards to the women themselves — a subject largely ignored in occupational health.
 HEALTH INDUSTRY
HEALTH INDUSTRY
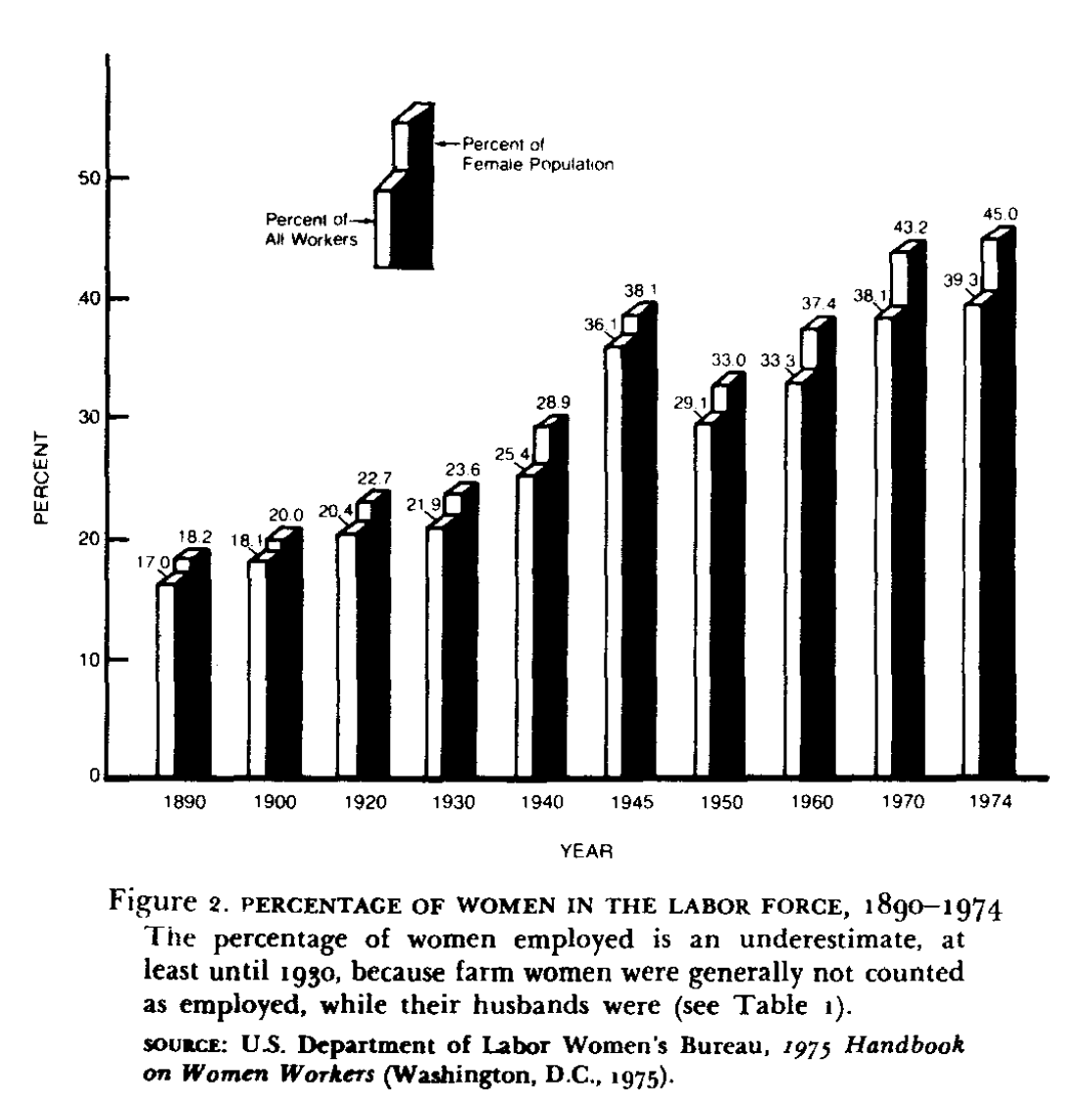
Health care is a huge, labor-intensive industry, employing over three million women. Over 70 percent of health workers are women; of these, 20 percent are registered nurses and more than half are service workers — nurse’s aides, food handlers, and janitors (see Figure 4). While health workers face an extraordinary variety of hazards ranging from ozone exposure, to x-rays, to laser beam lesions, a few examples of hazards — hepatitis, back injury, and heat stress — will serve to illustrate typical problems.
Infectious Diseases
It’s not surprising that nurses (97 percent of whom are women) suffer an abnormally high incidence of serious infectious diseases, including hepatitis, tuberculosis, staphylococcus, herpes simplex, and Rubella (German measles). But direct patient contact is only one means of exposure; also at risk are workers who transport, analyze, and dispose of biological specimens, including laboratory and janitorial workers.
A recent survey of hepatitis risk conducted by Local 1199 of the National Union of Hospital and Health Care Employees showed that laboratory workers in 34 New York City hospitals experienced more than twice the incidence of hepatitis found in the general population. (This study may be applicable to the nation’s 200,000 clinical laboratory workers, of whom 74 percent are women.) The survey implicated mouth pipetting as one major reason for high hepatitis risk. This practice is dangerous. Pipettes are strawlike tubes used to transfer liquids, often used for blood, urine, and other biological samples. Those workers who accidently had taken a mouthful of liquid — even once — had nearly three times the hepatitis risk of workers who claimed they had not. Automatic pipettes are not routinely provided in most hospital labs. Inadequate methods of specimen disposal and poorly packaged and labeled specimens also cause contamination problems. The risk of hepatitis is high as well among kidney dialysis workers, dentists, and persons working with drug abusers. Due to a lack of research concerning the spread of hepatitis and other diseases, the true extent of hospital induced infections among staff and patients is not known.
Hospital Service Workers
Hospital service workers have the dirtiest and least rewarding work. They must lift patients and carry loads of food service or cleaning equipment, making back injuries a major recognized hospital problem. Although it is unsafe for an unassisted worker to lift a patient, hospitals continue to employ so few workers that teamwork is made impossible. Other preventive measures such as mechanical carrying devices and better bed design have not been instituted.
Very little attention has been paid to the health and safety of the many hospital service workers employed in laundries. Counting both in-hospital and outside laundries, the number of employees is 350,000 — 70% are women.
Laundry work is dangerous and hard. The temperature and humidity are often unbearable, taking a toll on the cardiovascular system. It is well known that heat causes an increase in blood flow to various organs and can lead to acute reactions such as heat stroke and liver damage. However, we can only guess the long term health costs from thermal stress. The need for research is especially striking because heart and circulatory disease have become leading causes of death.
Laundry equipment is frequently poorly designed and maintained, exposing workers to burns, electric shock, and severe injury from unguarded machinery. Another hazard is exposure to dangerous substances in the laundry. In hospitals, hepatitis and other diseases have been transmitted in this way. (Outside hospital laundries, cases of silicosis — and asbestos-related diseases have been recorded among persons washing dusty work clothes.)
In conclusion, the general industrial and physical dangers facing hospital workers are compounded by the exposure to pathogens (communicable diseases) and to biologically active agents (disinfectants, anasthetics, x-rays). Rapidly developing technologies in medicine assure new sources of hazards for health care workers.
CLERICAL WORKERS
Little attention has been paid to the health hazards of clerical work. As more than one out of every three working women is employed as a clerical worker (compared with less than one of every ten working men), this is an oversight which represents a serious problem for women. Traditionally, the health and safety of workers has been taken seriously only after tragedies have come to light — like deaths from accidents or cancer. Even then, regulation of these hazards is often inadequate.
The fact that clerical workers are not exposed to immediately life-threatening dangers does not mean that their work is free from hazards. And office workers, like all other workers, have the right to a safe and healthful workplace, guaranteed by law.
There is still much to be learned about hazards for clerical workers, but some dangers are already known. They include:
- Sitting all day, which can lead to back problems, hemorrhoids, varicose veins, and other circulatory problems.
- Exposure to toxic solvents which are used for duplicating machines and found in common office supplies, like rubber cement.
- Exposure to ozone from duplicating machines in poorly ventilated places.
- Exposure to asbestos in the air conditioning.
- Stress (both physical and emotional) which can result in serious health problems, ranging from daily headaches to ulcers and high blood pressure.
Seating
Backaches appear to result from poorly designed chairs. They can be aggravated by the stress that often accompanies “sit-down” jobs. Unfortunately, executives usually get the best chairs, secretaries the worst ones although they spend more time in them. Poor chairs also impede circulation, thereby causing or aggravating varicose veins and hemorrhoids.
Lighting
Some people cannot work under fluorescent light without suffering severely from impaired vision, swollen eyelids, and bloodshot eyes. The flicker and hum can also be disturbing, possibly causing headache and fatigue. Persons predisposed to epilepsy may even be triggered into a seizure by the light.
Fluorescent lights are known to leak a small amount of x-rays. Whether these levels are dangerous over a long period of exposure is not known.
VDT’s: A New Hazard
Modern technology has invaded the clerical world in the form of video display terminals (VDT’s). Millions of these machines are used by workers in publications, communications, banks, law offices, and retail stores. The VDT’s look like electric typewriters attached to a television screen. VDT’s are powered by cathode ray tubes, an artificial illumination source, similar to that found in televisions or fluorescent lights.
In 1976, two male copy editors at the New York Times developed cataracts after they started working with VDT’s. Seventy-five United Nations typists later walked off their jobs, refusing to work on VDT’s, citing health dangers. The most immediate problem is eye-strain. Additional complaints include visual deterioration, headaches, fatigue, and backaches. Whether some of these complaints are related to the machines or other conditions of work is not known.
In sum, it is apparent that clerical work is not “safe,” as is commonly presumed. In fact, hazards are prevalent, sometimes aggravated by new mechanical and chemical additions to the workplace. These issues are rarely the target of union activity or scientific research.
BLUE COLLAR WORKERS
Fifteen percent of women workers are in blue collar jobs. They are highly concentrated in either a few industries, such as clothing and textiles, or in certain parts of industries, such as circuit board assembly in the electronics industry. While hazards women face in these jobs are not known to affect women selectively, workplaces dominated by women are not the usual focus of industrial health research nor are the kinds of hazards borne by female industrial laborers ordinarily public knowledge. Additionally, changes in the chemical complexity of traditional women’s industrial jobs have dramatically intensified the chemical dangers of what once might have been considered benign “women’s work”.
Textiles
To give some index of the concentration of female workers in the textile industry, 94 percent of the stitchers and sewers in the clothing industry are women (875,000 women workers). Another 500,000 women (76 percent of this labor force) are employed as manufacturers of fabricated textile products and apparel.
Serious workplace hazards which women in the textile industries face relate in part to problems arising from the use of natural and synthetic fibers and to changes in the treating, assembling, and finishing of fabrics. Women who work with cotton, for example, are exposed to cotton dust which in turn can produce byssinosis, a disabling lung disease commonly known as “brown lung.” No specific estimates have been made of the number of women workers with brown lung, but the Public Health Service estimates that 500,000 workers currently have brown lung disease. These workers, most of whom live in the southeastern United States, are forced to leave their jobs after contracting the disease, and usually — because most cotton mills are nonunion and function without health benefit programs — these workers receive no compensation for their disability.
Replacement of cotton and other natural fibers by petroleum-based synthetics, and development of new methods for assembly and treatment of fabrics, have resulted in exposure of workers to new chemical dangers. Polyester basting threads are now removed by solvents, thereby exposing the stitchers and sewers to the toxic fumes of complex chemical reactions. There is also evidence that Tris, the chemical flame retardant impregnated into certain fabrics before it was banned as a suspected carcinogen, was absorbed through the skin of garment workers. Unfortunately (perhaps conveniently), research on this problem was dropped when Tris was banned. There is also evidence that the potent carcinogen BCME (bis-chloromethyl ether) may form spontaneously from the interaction of formaldehyde residue from permanent press fumes with acidified chloride ions often present in textile processes.
Cosmetology
New complex chemicals have also dramatically invaded the workplace of cosmetologists, barbers, and hair dressers. Almost 450,000 (68 percent) of these jobs are held by women. These women risk respiratory disease because of the extensive use of aerosol, volatile dyes, detergents, solvents, and lacquers. There is some evidence they also may be at risk for cancer in the use of hair dyes.
Electronics
About 115,000 women work in the assembly and manufacture of electrical machinery, equipment, and supplies. They constitute 55 percent of the electronics labor force but are disproportionately involved in the assembly of printed circuit boards, a task which requires soldering miniature components. While soldering, these women inhale cadmium fumes, a metal present in the solder flux. Cadmium has been associated with a number of health problems including: weakness, nausea, vomiting, rapid pulse, inflammation of lungs, cough, soreness of chest, “metal fume fever,” chemical pneumonitis, emphysema, kidney damage, and cancer. Circuit board assemblers are also routinely exposed to solvents such as trichloroethylene, a compound which has been found to cause cancer in test animals and is suspected of causing liver damage.
Conclusion
What do working women have to look forward to? Changes in production technology in the industries where women are employed (such as health care, textiles, clerical and electronics) continue to create new health dangers. More and more, women face the added stress of the dual role: homemaker plus breadwinner. And they can’t just quit work and go home; most employed women work out of economic need. These trends look like they will continue.
Reporoductive Health Rights of WorkersSome Facts
Some Misconceptions
|
But worthwhile reforms are possible; during World War II, when it was essential to bring women into the work force, childcare centers, flexible shift jobs, and job sharing made it easier for homemakers to take jobs. Other gains have been permanent. A minimum wage, the eight hour day, and overtime pay were first granted to women and then extended to all workers. Although these advances were originally justified by sexist generalization about the “weaker sex,” they have been positive steps in the fight for occupational health and safety. Recently industry has tried to exclude women from certain jobs on the pretext of reproductive health standards. Keeping women on these jobs and insisting that they be made safe may result in further advances in workplace conditions for both sexes.
Unions remain the best tool in fighting for occupational health. Organizations like Union Women’s Alliance to Gain Equality (Union WAGE) and Women Office Workers (WOW) have been active in helping women unionize. This is a two part movement, both to gain equality in existing unions and to create unions in presently unorganized fields such as electronics and office work.
We must oppose attitudes that see women’s work roles as unimportant and their jobs as inherently safe. Industry profits from these attitudes, justifying poor working conditions and low pay, literally at women’s expense.
RESOURCESWomen’s Occupational Health Center: Collects and interprets scientific literature related to occupational health concerns of women. Publishes a newsletter, a quarterly Technical Bulletin, and informational packets. Write to: American Health Foundation, 320 East 43rd St., New York, NY 10017. Union Women’s Alliance to Gain Equality (Union WAGE): Organizes around women’s issues and publishes a newsletter. Write to: P.O. Box 40904, San Francisco, CA 94140. |
>> Back to Vol. 12, No. 2 <<
BIBLIOGRAPHY
Jeanne M. Stellman, “Occupational Health Hazards of Women: An Overview,” Preventive Medicine, vol. 7, 1978, pp. 281-93.
Stellman, “The Hidden Health Toll, A Cost of Work to the American Woman,” Civil Rights Digest. Fall 1977, pp.32-41.
Stellman, et al., “The Role of the Union Health and Safety Committee in Evaluating the Health Hazards of Hospital Workers: A Case Study,” Preventive Medicine. vol. 7, 1978, pp. 332-37.
Stellman, Women’s Work, Women’s Health (New York: Pantheon Press, 1977).
Stellman and Susan M. Daum, Work is Dangerous to Your Health (New York: Vintage Books, 1973).