This essay is reproduced here as it appeared in the print edition of the original Science for the People magazine. These web-formatted archives are preserved complete with typographical errors and available for reference and educational and activist use. Scanned PDFs of the back issues can be browsed by headline at the website for the 2014 SftP conference held at UMass-Amherst. For more information or to support the project, email sftp.publishing@gmail.com
Blaming the Victim: Hyperactivity & Social Control
by Patty Bronson
‘Science for the People’ Vol. 9, No. 5, September-October 1977, p. 20–24
While addressing a conference on “The New Nutrition,” Dr. Benjamin Feingold stated: “As many as seven million children have been diagnosed as having serious learning problems. About five million are considered hyperactive. At least two million are being treated with drugs, usually Ritalin or amphetamines, in an attempt to control their wild behavior. No one expects these drugs tb cure hyperactivity. All they can do is mask it and they might be doing much more. They are certainly making zombies out of a goodly percentage of the younger generation.”*1
Peter Schrag and Diane Divoky, in their book The Myth of the Hyperactive Child, describe the development and increasing use of psychosocial and psychochemical techniques, based on an ideology of “early intervention” which regards almost every form of undesirable behavior as a medical ailment requiring medical treatment. The acceptance of such an ideology by doctors, parents, drug companies, children, teachers, health professionals and school officials has profound implications for our entire society.
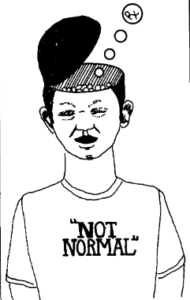
In 1957, Maurice Laufer announced the discovery of a new syndrome which he called “hyperkinetic impulse disorder.” The most striking symptom of the disorder was hyperactivity. “The sickness, in brief, was the inability to function in school. “2 Symptoms include a short attention span, impulsiveness, irritability, explosiveness, poor powers of concentration, and poor school work. Definitions of the term hyperkinesis have become increasingly vague. The term now includes virtually all forms of social and academic nonconformity.
Through the work of Sam Clements and his task force at the University of Arkansas Medical Center, in 1966 a new label, Minimal Brain Dysfunction (MBD), was chosen for “clarification” of this disorder. MBD is an encompassing term which covers hyperkinesis, hyperkinetic behavior disorder, functional behavior problems, overactivity, hyperactivity, cerebral dysfunction and up to thirty other terms. In explaining the choice of words, Schrag and Divoky say, “The ‘minimal’ indicated the absence of extreme behavior and ‘dysfunction’ was used to get around the necessity of finding an organic problem.”3

Despite volumes of basic research and clinical observation, hyperkinesis is still not understood. An HEW panel reported that “the major symptoms are an increase of purposeless physical activity and a significantly impaired span of focused attention.”4 They also concluded that there is no known single cause of the disorder. Although most of the names listed above suggest brain damage, virtually all symptoms of MBD are behavioral. No current neurological test or combination of tests can differentiate hyperactive or MBD children from “normal” children. “The only advance made during the past ten years has been the recognition that the hyperkinetic syndrome does not necessarily indicate organic brain damage. “5 As many as 300 possible MBD symptoms have been identified to date. These symptoms are so general that any child might exhibit any of them. The following list is a part of the “clarification” literature presented by Sam Clements and his task force some years ago:
“spotty or patchy intellectual deficits,” “achievement low in some areas, high in others,” “hyperkinesis” or its opposite “hypokinesis,” “general awkwardness,” “slowness in finishing work,” “reading disabilities,” “arithmetic disabilities,” “poor printing, writing, or drawing ability,” “easy fatigability,” “peer group relationships generally poor,” “thumb-sucking, nail-biting, headbanging, and teeth-grinding in the young child,” “slow to toilet train,” “explosive,” “sleep abnormally light or deep,” “physically immature, or physical development normal or advanced for age,” “possibly antisocial behavior,” “possibly negative and aggressive toward authority,” “sweet and eventempered, cooperative and friendly,” “impaired ability to make decisions, particularly from many choices.”
It is obvious that hyperkinesis (hyperactivity or MBD) does not have a very precise and distinct clinical meaning. But in spite of its obvious faults, the Clements work became a staple in educational theory and legitimized the diagnosis of MBD. It is estimated that anywhere from 15 percent to 40 percent of our children are labeled as “learning disabled” or “hyperactive.” The extensive literature never clarifies what exactly we are dealing with here. I am extremely concerned because up to two million children today are being “treated” for this so-called disease, with medication whose safety is questionable.
There are several different approaches used for treating children diagnosed as having MBD. These include educational, recreational, medical or psychological treatment, or some combination of these. Even though very few children have a problem serious enough to require chemotherapy (the use of behavior-modifying drugs), it is the most common method of treatment. Ritalin is the most commonly prescribed of the stimulant drugs; other such drugs include Benzedrine, Mellaril, Dexadrine and Thorazine. The use of these psychoactive drugs to modify behavior has become a standard medical practice. However, it should be made clear that “drug therapy neither cures the child nor corrects the cause of the behavioral disturbance.”6 It does not get to the root of the problem. In addition, no long-term studies have been done which unambiguously demonstrate that this therapy is safe over extended periods of time. It seems to be generally accepted that chemical therapy allows the child to “conform” or “maintain” within the system which decided that he or she is somehow abnormal. Doctors, teachers, and parents report that the stimulants help children sit, concentrate and learn without making them sleepy or “dopey.” It is thought that drug treatment can improve the child’s self-esteem and the attitudes of teachers and parents toward the child.
There are numerous risks involved in the use of these drugs and these should be seriously considered. Such treatment may cause psychological damage in as much as the child comes to see Ritalin or another drug as the magic pill that makes his or her behavior good. But where do standards of ‘good’ come from? Perhaps the child was only disturbed or bored by a teacher or classroom situation. The possible connection between childhood dependence on behavior-modifying drugs and drug abuse in later life is not yet understood. There is always the risk that the children, doctors and parents involved will come to see the medication as a cure-all. Alternative solutions are often ignored and efforts of adults to understand the child and help by other means may be lost when behaviors are masked.
Ritalin (methylphenidate), marketed by Ciba Pharmaceutical Co., is classified as a stimulant and is related to the amphetamines. The action of the drug on brain chemistry is not fully understood, but it has been know since 1937 that stimulants can produce a “subduing effect” on children. Ritalin falls under Schedule II of the Controlled Substances Act, the most restricted classification for marketed drugs. It is regarded by the FDA and the Bureau of Narcotics and Dangerous Drugs as a “dangerous drug.” According to John Finlator, deputy director of the Bureau of Narcotics and Dangerous Drugs, Ciba produced 334,000,000 dosage units of Ritalin in 1970.* Since 1972, federal regulations have prohibited the drug companies from promoting products like Ritalin directly among parents and teachers. ‘The regulations do not, however, prevent the firms from promoting the ailment or from defining it in the broadest possible terms, a process that is reinforced by the extensive set of relationships between the drug companies, certain doctors and research teams, and the lay movement.”7 While we don’t know how extensive these connections are, or the amounts of money involved, it is in the interests of the drug companies to promote the existence of the disease and thus a market for their product.
Treatment with behavior-modifying drugs provides only symptomatic relief of the “problem behaviors.” The duration of the treatment varies from 6 months to 6 years. Some believe these drugs are probably among the safest ever discovered; when used in medical dosages they are said to have essentially no major toxic effects.
The 1973 edition of the Physician’s Desk Reference disagrees:
Ritalin should be given cautiously to emotionally unstable patients. Nervousness and insomnia are the most common adverse reactions but are usually controlled by reducing dosage and omitting the drug in the afternoon or evening. Other reactions include hypersensitivity including skin rash, urticaria, fever arthralgia, exfoliative dermatitis, and erythema multiforma with histopathological findings of necrotizing vasculities, anorexia, nausea, dizziness, palpitations, headache, pulse changes (both up and down), tachycardia, angina, cardiac arrythmia, abdominal pain, weight loss. During prolonged therapy, insomnia and tachycardia may occur more frequently. Toxic psychosis has been reported.
While many physicians now recognize the dangers in prescribing amphetamines for overweight adults, most continue to use them for hyperactive children. Sometimes a “problem child” will be allowed to return to school only if he or she takes medication. This practice takes place despite the absence of adequate longterm and controlled studies of MBD children.
Those studies which have been done “do not show long-term or lasting improvement in behavior or learning from the use of Ritalin. “8
 The problem is not merely medical: Who should be responsible for labeling these children? Where in actuality are the diagnoses coming from? Is it right to categorize them at all? Is mischief abnormal? What are the responsibilities of a school system? Are the alternatives to drug therapy being lost in a drug-oriented society? All these questions take us out of the realm of medicine and into the realm of politics. Is the child becoming the scape-goat for the social and psychological ills in certain families and classrooms? Will he or she become obedient and docile in order to escape being drugged? Should they submit to regimentation? Have our tranquilizers dulled our sensitivities so much that we are freaked out by childlike innocence, excitement and curiosity? Is it the aim or our educational system to mass-produce unquestioning, docile, accepting little beings? Have we finally found it necessary to suppress human growth? These, of course, are not clinical questions. They are, however, reasonable questions to raise.
The problem is not merely medical: Who should be responsible for labeling these children? Where in actuality are the diagnoses coming from? Is it right to categorize them at all? Is mischief abnormal? What are the responsibilities of a school system? Are the alternatives to drug therapy being lost in a drug-oriented society? All these questions take us out of the realm of medicine and into the realm of politics. Is the child becoming the scape-goat for the social and psychological ills in certain families and classrooms? Will he or she become obedient and docile in order to escape being drugged? Should they submit to regimentation? Have our tranquilizers dulled our sensitivities so much that we are freaked out by childlike innocence, excitement and curiosity? Is it the aim or our educational system to mass-produce unquestioning, docile, accepting little beings? Have we finally found it necessary to suppress human growth? These, of course, are not clinical questions. They are, however, reasonable questions to raise.
The basic problems, as viewed by a group of health professionals, teachers and other concerned citizens from New York City, are: 1) schools which do not meet the needs of children, 2) drug-manufacturing companies that are too eager to sell their products and 3) doctors who treat all problems with drugs. Most medical groups endorse the use of amphetamines for hyperkinetic children. A notable exception is the American Academy of Pediatrics, which lists three fundamental problems associated with the use of these behavior-modifying drugs 1) no uniform, agreed-upon terminology to describe these disorders; 2) “marked variability in the methodology for evaluation” (there is also no consistent way o’r determining whether a given treatment is effective) and 3) “the absence of standardized requirements for precise diagnosis and classification of the symptomatology constituting impediments.” The use of behavior-modifying drugs suggests to parents and children that there can be a chemical solution to learning, interpersonal and societal problems.
Dr. Ben Feingold of the Dept. of Allergy of the Kaiser-Permanente Medical Center in San Francisco has suggested what seems to be a promising alternative to drug therapy for hyperactive children. Observations have implicated food additives as a partial cause in hyperkinesia. “A federally funded study has confirmed that removing artificial flavors and colors from foods can indeed reduce hyperactivity in susceptible children.”9 A recent double-blind study* also showed positive results. Feingold’s special elimination diet excludes all artificial food dyes and flavorings. However, this is an ali-or-nothing diet. A child who takes a single bite of an artificially flavored or colored food will trigger a reaction within a few hours that may take several days to subside. That reaction is generally the recurrence of the original hyperactive “behavior.” Feingold proposes that a symbol appear on all food and beverage packages to indicate the complete absence of artificial colors and flavors. “A program of strict dietary adherence should be rewarding in about 50 percent of the H-LD (hyperkinesis and learning disabilities) children. Once a favorable response is observed, both parents and child become aware that not only the cause for the behavior is known, but that a cure is available, too.”10
It is necessary to be aware of alternatives not only in treatment but in attitude. There are many questions not touched on here which may trigger concern in a community. People need to be educated about the problems of diagnosis and treatment of MBD. We also need to look at the relationship between MBD and the values of the American educational system. There are also simple practical considerations for parents who have a child diagnosed as “hyperactive.” Before allowing their children to be drugged, they should consult and question advisors, family workers, psychologists or social workers who may be able to offer alternative solutions.
My feelings on this subject are strong and my intent has been to raise questions, and suggest the need for a reevaluation of the problem. Beyond the technical issues, there is a human concern for every child as an individual.
* Dr. Feingold has implicated food additives as a partial cause of hyperkinesia and has successfully treated children with a salicylate-free diet. ↵
* Abbott Laboratories has invested $10 million in “Cylert,” a new drug now ready for marketing for use on MBD children. ↵
* Double-blind study: a study in which an alternative drug (or a placebo, which has no effects at all) is used as well as the drug being studied, and neither the investigator nor the child know which is being taken. ↵
>> Back to Vol. 9, No. 5 <<
REFERENCES
- “Proof of the Feingold Thesis,” Prevention, December 1975, p. 57.
- Divoky, Diane and Peter Schrag, “The Invention of a Disease,” Edcentric, issue no. 35, July-August 1975, p. 23.
- Ibid., p. 8.
- Haar, T.A. Yonder, “Chaining Children with Chemicals,” The Progressive, March 1975, p. 13.
- Feingold, Ben F., “Hyperkinesis and Learning Disabilities Linked to Artificial Food Flavors and Colors,” American Journal of Nursing, Vol. 75, No.5, May 1975, p. 798.
- Ibid., p. 800.
- Divoky and Schrag, “The Invention of a Disease,” p. 24.
- “Schools, Doctors and Drugs,” The Medical Committee for Human Rights, p. 2.
- “Proof of the Feingold Thesis,” p. 56.
- Feingold, “Hyperkinesis and Learning Disabilities,” p. 803.